We conducted our first round of polling in India and Kenya in late November 2020. At the time, both countries had managed to avoid the worst of the pandemic’s effects. Fast forward six months to our second round of polling (May 10-18, 2021), and India was at the height of a crushing wave. The COVID-19 vaccine roll-out was also underway in both countries.1
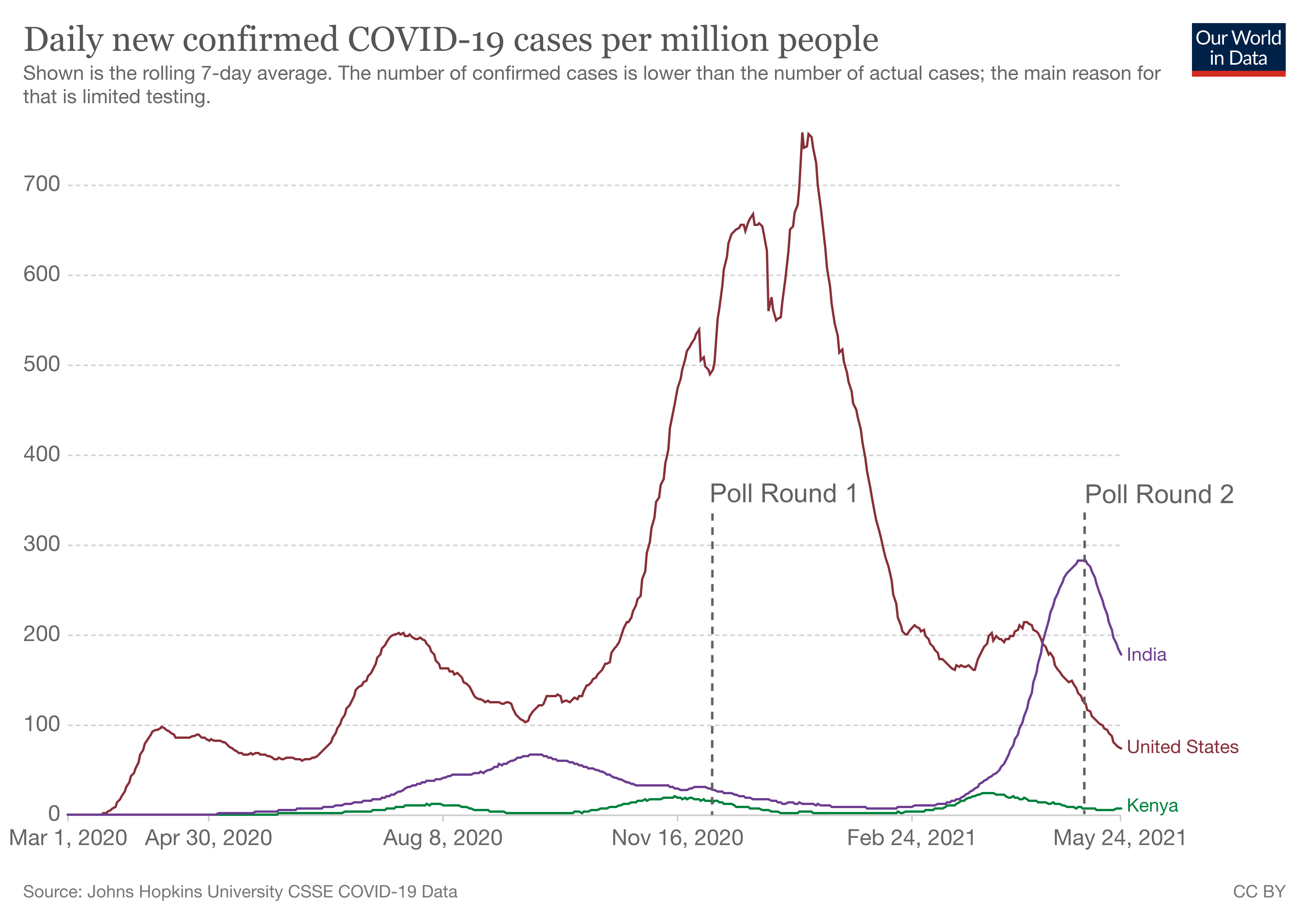
Figure 1: Daily new confirmed COVID-19 cases per million people. Data from JHU CSSE. Graph by Our World in Data, https://ourworldindata.org/covid-cases.
Methodology
For these polls, we relied on digital marketing and did not run any offline campaigns (e.g., billboards, fliers, radio) in the interest of time. Facebook users saw our ads in their timelines (Facebook or Instagram),2 and clicking on an ad opened a chat in Facebook Messenger or WhatsApp. This started an automated conversation with the askNivi chatbot.
Figure 2: LEFT: Example Kenyan ad from November 2020. RIGHT: Example Indian ad from May 2021 (‘Have you received a COVID-19 vaccination yet?’).
Nivi asked users to select a language (English or Swahili/Hindi), provide basic demographic information, and answer a few topline questions. Users who agreed to continue could answer several additional questions. We used multilevel Bayesian regression and post-stratification to adjust the results. See the technical notes below for details.
What We’re Learning
Concern about COVID-19
We estimate that more than 8 out of 10 people in both countries are somewhat or very concerned about COVID-19. This represents an increase of 9 percentage points in India since November, +6 pp in Kenya.
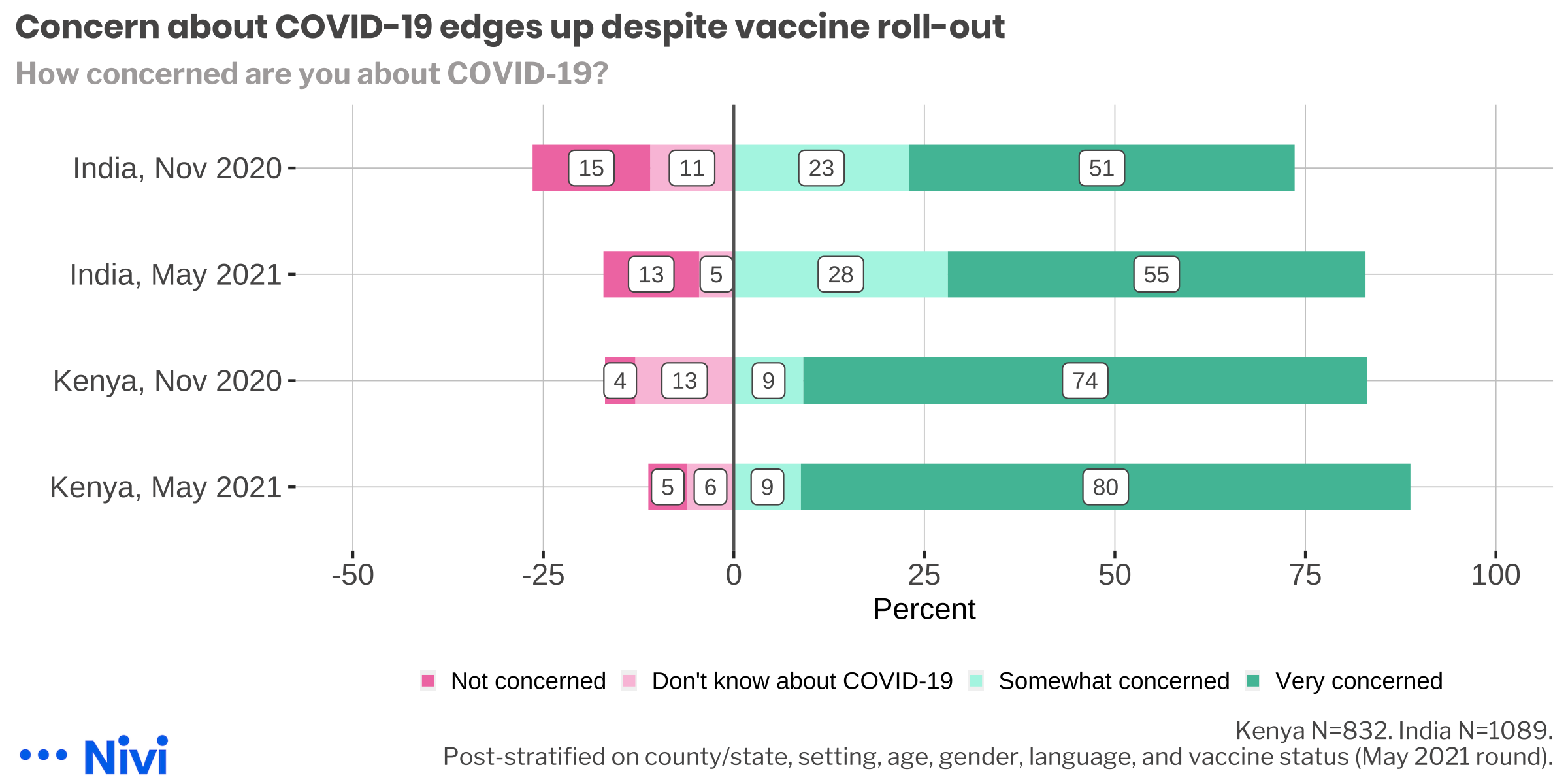
Figure 3: Concern about COVID-19
This increase in concern about COVID-19 was observed across demographic groups. Men in India and young people in Kenya saw the biggest jumps.
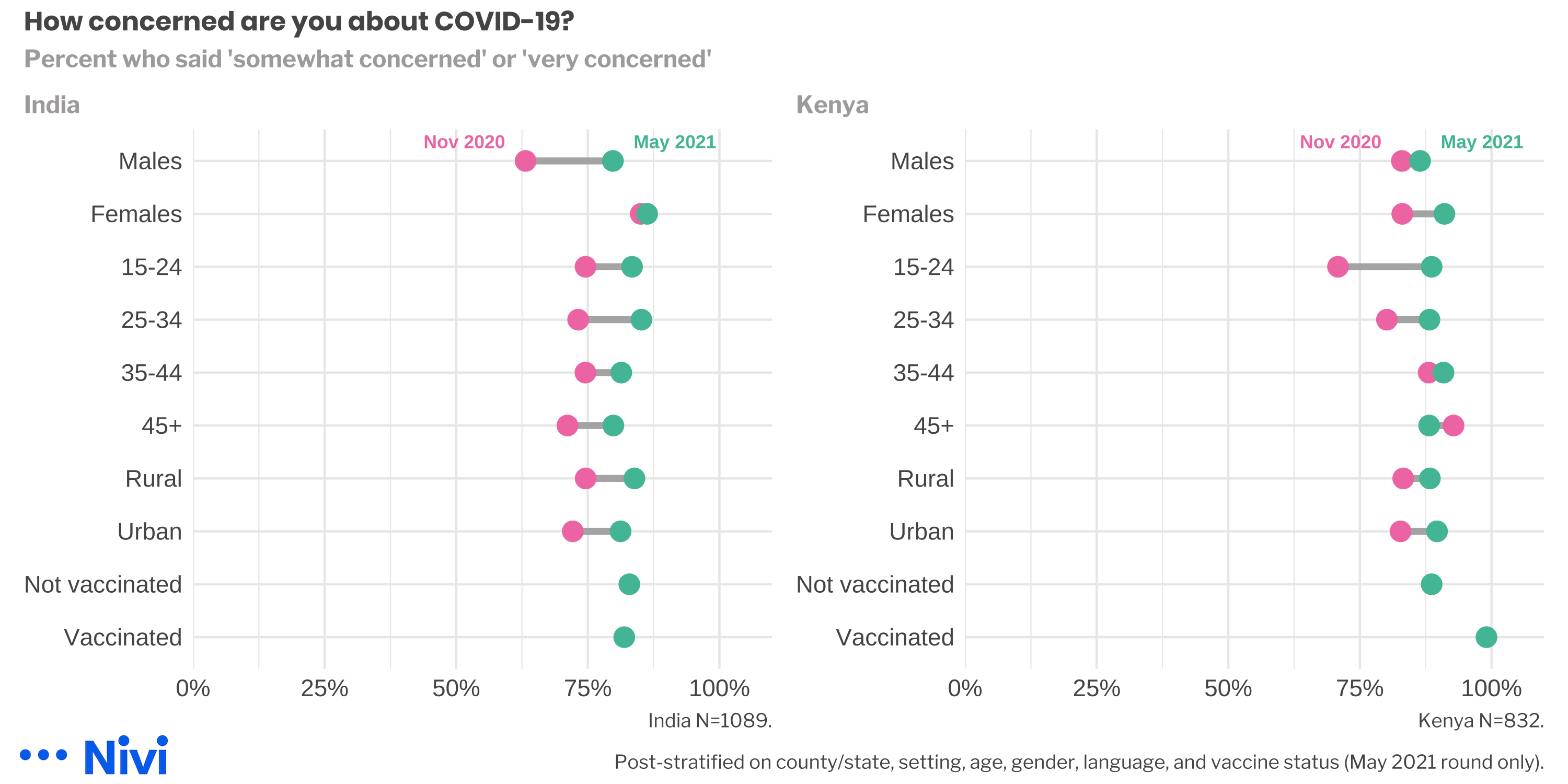
Figure 4: Concern about COVID-19 by country and background characteristics.
Self-reported mask wearing around non-household members remains high in both countries, though we observed a big jump in India in May.
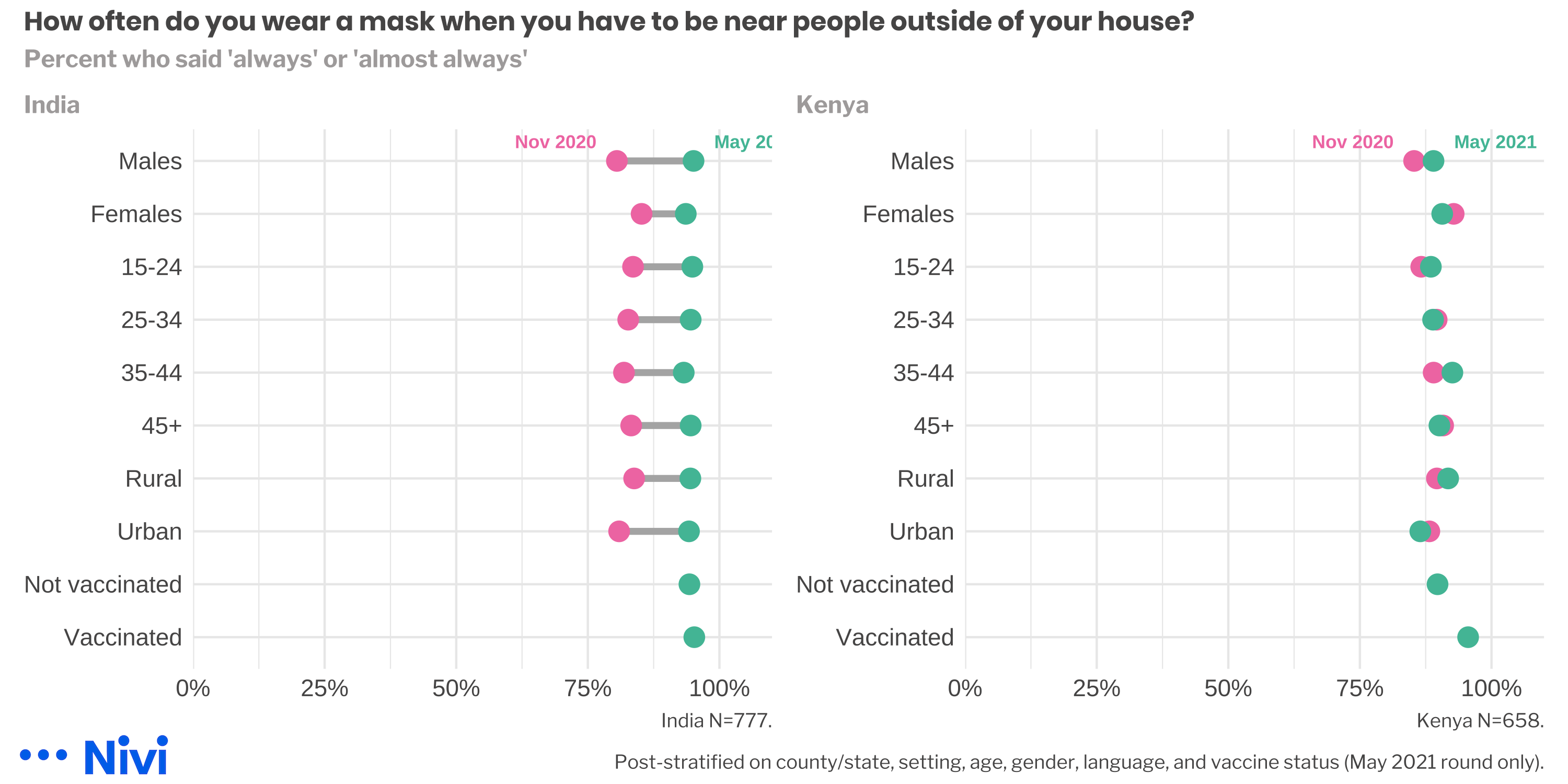
Figure 5: Mask wearing by country and background characteristics.
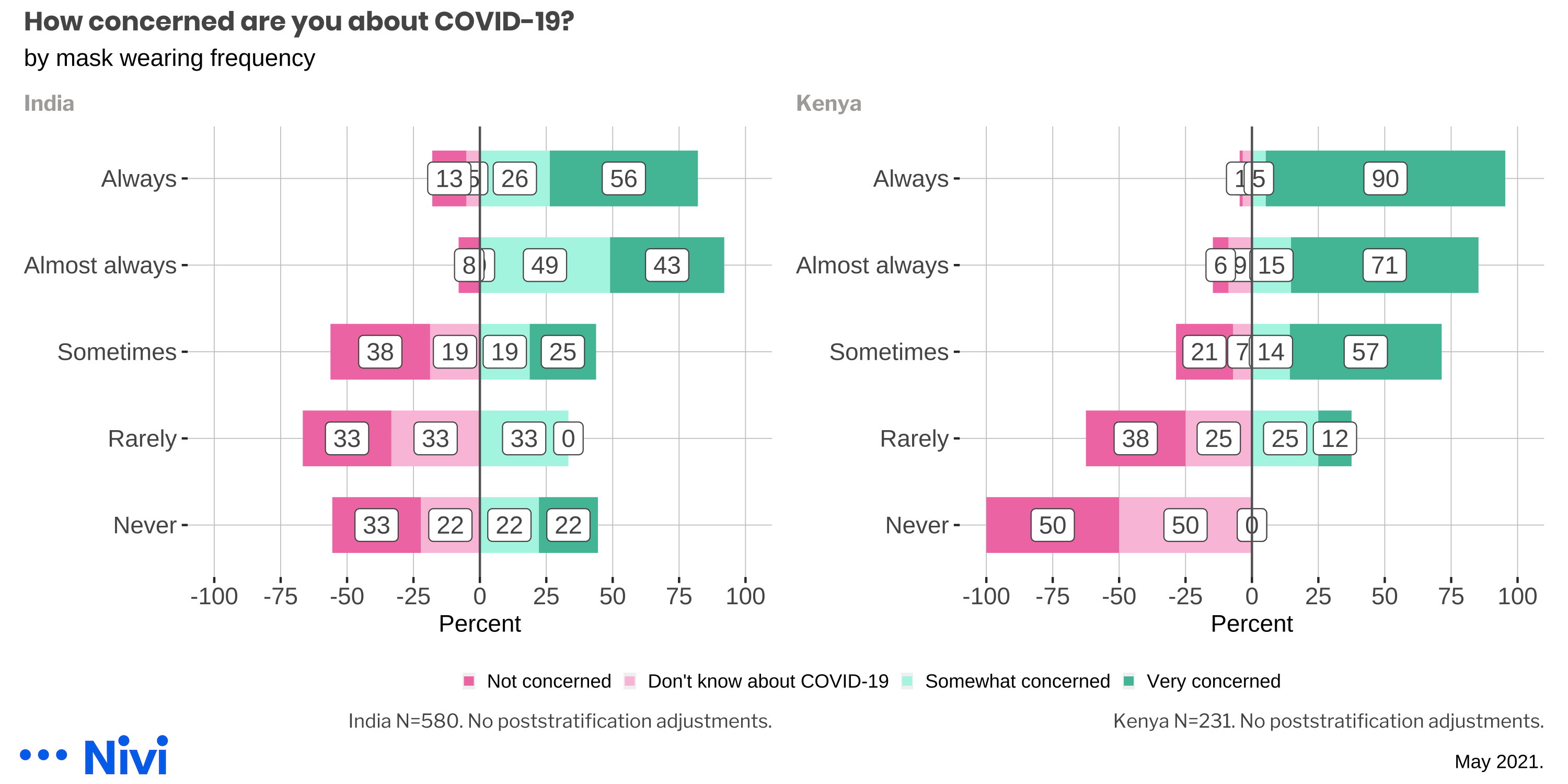
As you might expect, taking precautions like wearing a mask when it’s not possible to socially distance from non-household members is associated with one’s perceptions about the seriousness of the pandemic. This pattern is most apparent in Kenya.
Despite being an internet sample, most Kenyan respondents said they get news about the pandemic from traditional media sources, such as radio, TV, and newspapers. In India, half of respondents said they turn to the internet instead.
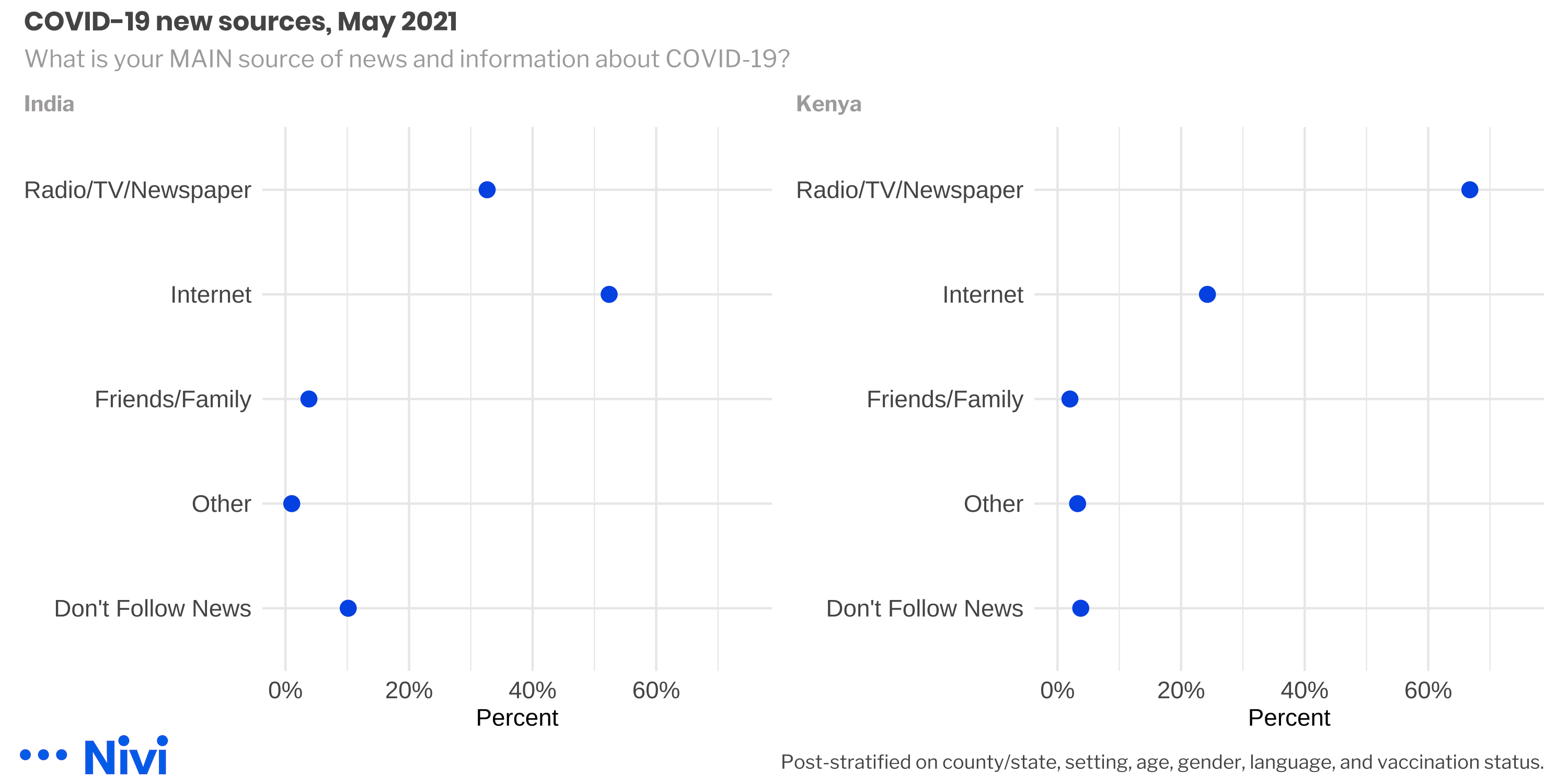
Figure 6: What is your MAIN source of news and information about COVID-19?, May 2021
Vaccine Hesitancy
We estimate that COVID-19 vaccine hesitancy in Kenya has held steady in the 10% to 25% range since November. In India, however, we detected a sharp decline in hesitancy in May at the (possible) peak of the current wave of COVID-19 cases.
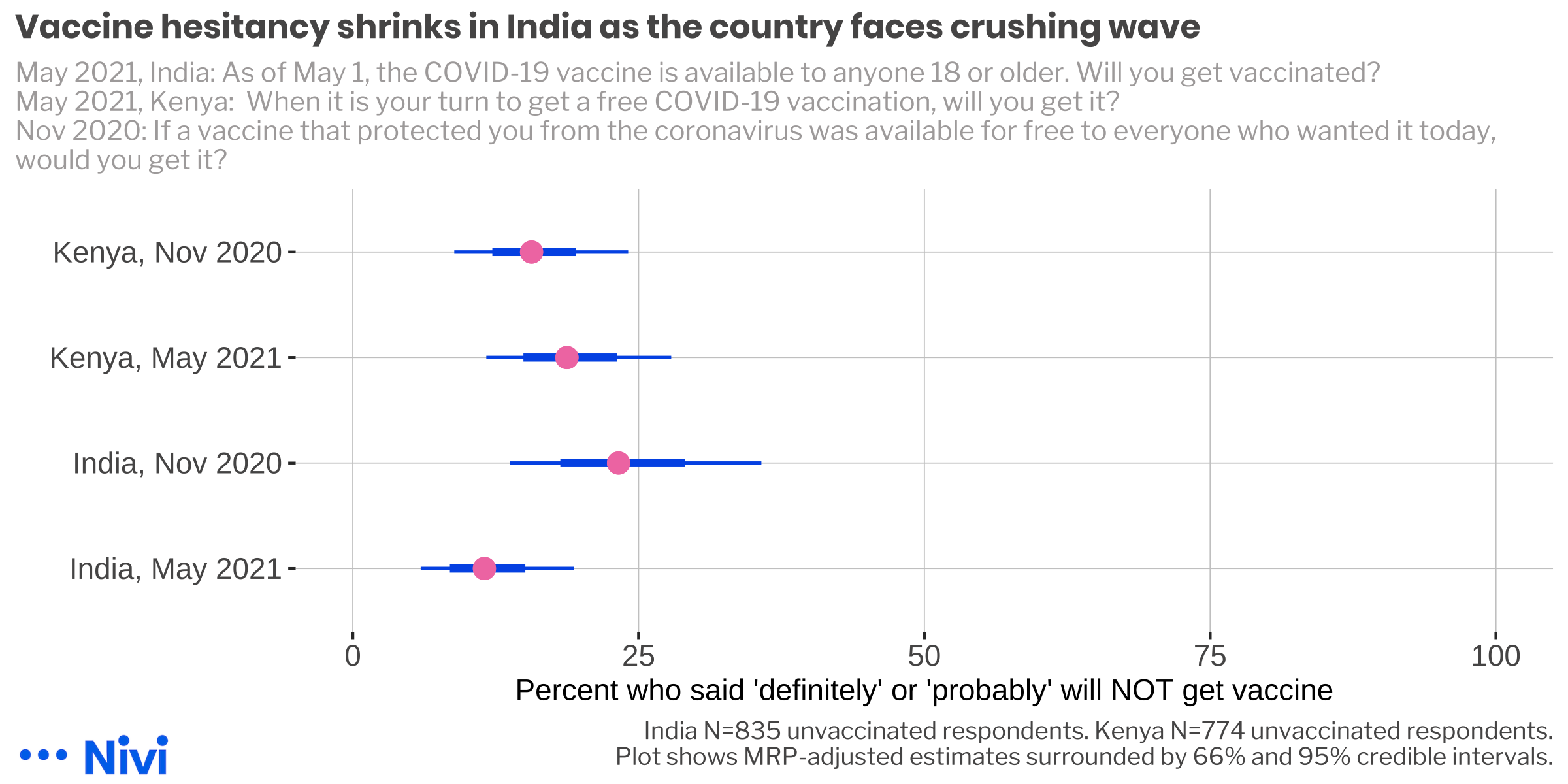
Figure 7: COVID-19 vaccine hesitancy.
Our November 2020 estimates appear to track with other polls with the exception of a SMS survey conducted by GeoPoll.
| Estimates of COVID-19 vaccine hesitancy | ||||||
|---|---|---|---|---|---|---|
| Percent | Country | Period | Organization | Channel | Method | N |
| 25 | India | Jun 2020 | Lazarus et al. (2020)1 | multiple international online panel providers | randomized stratified sampling from existing panels | 742 |
| 29 | India | Apr 2020-Feb 2021 | Ideas for India2 | Facebook COVID-19 Symptom Survey (CSS) | convenience, adjusted | 277844 |
| 23 | India | Nov 2020 | Nivi | convenience, adjusted | 309 | |
| 12 | India | May 2021 | Nivi | convenience, adjusted | 469 | |
| 14 | Kenya | Oct 2020 | Statista3 | Computer-assisted telephone interviews | not stated | 1000 |
| 16 | Kenya | Nov 2020 | Nivi | convenience, adjusted | 544 | |
| 32 | Kenya | Nov 2020 | GeoPoll4 | SMS | sampling from existing panels | 500 |
| 19 | Kenya | May 2021 | Nivi | convenience, adjusted | 198 | |
|
1
https://www.nature.com/articles/s41591-020-1124-9
2
https://www.ideasforindia.in/topics/human-development/covid-19-vaccine-hesitancy-trends-across-states-over-time.html
3
https://www.statista.com/statistics/1221329/willingness-to-take-a-covid-19-vaccine-in-kenya/
4
https://www.geopoll.com/blog/covid-19-vaccine-sub-saharan-africa/
|
||||||
We do not observe any strong patterns to the hesitancy by background characteristics. In India, women and young people appear to be the most hesitant. In Kenya, however, we find men and users from urban areas are the most hesitant.
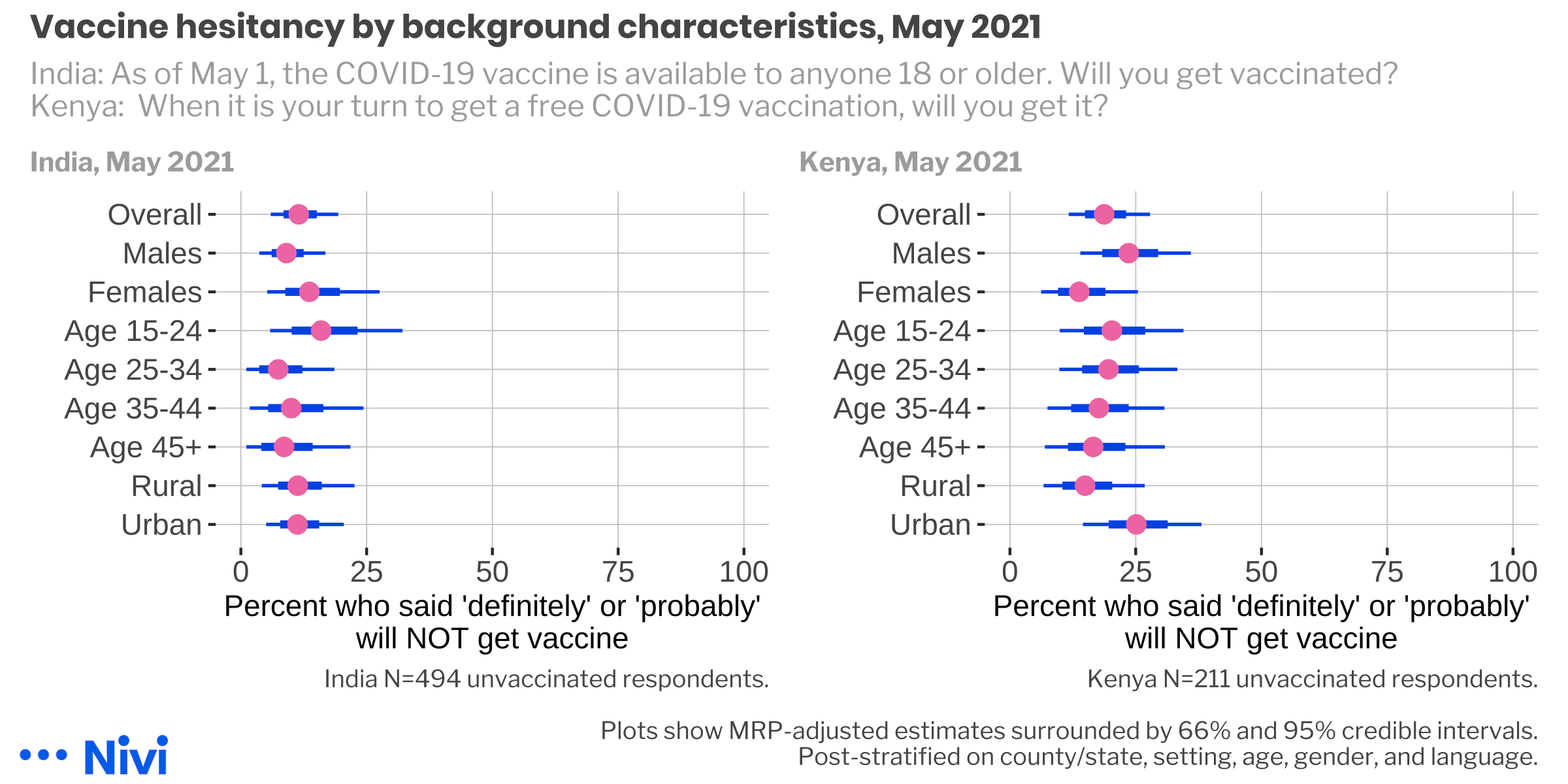
Figure 8: COVID-19 vaccine hesitancy by background characteristics, May 2021.
Understanding Hesitancy
We asked people who said they are not planning to get vaccinated to tell us the main reason why. The denominators are small (42 in India, 47 in India), so it’s important not to read too much into results, but we can think about the high-level trends as a starting point.
In both countries, the leading reasons were that people do not believe in vaccines and they have concerns about potential side effects. The most notable demographic difference might be that disbelief in vaccines seems to be strongest among women in both countries.
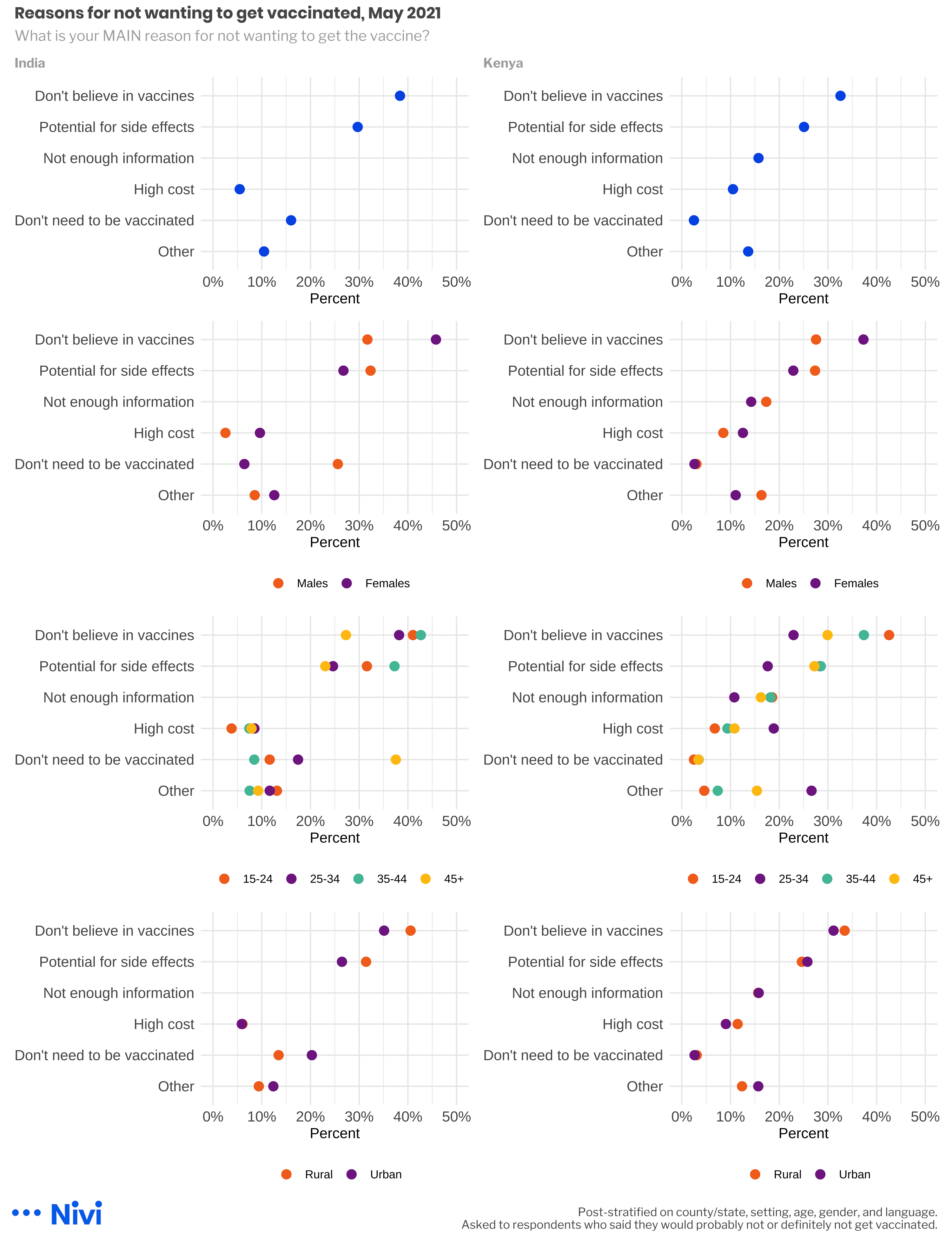
Figure 9: Main reason for not wanting to get vaccinated, May 2021
We also asked these respondents what they will look forward to most when the pandemic is over. The same caveats about small denominators apply here, too, but we can report that a large proportion said they look forward to business and the economy returning to normal. This might prove to be a useful hook in campaigns to convince the hesitant to get vaccinated.
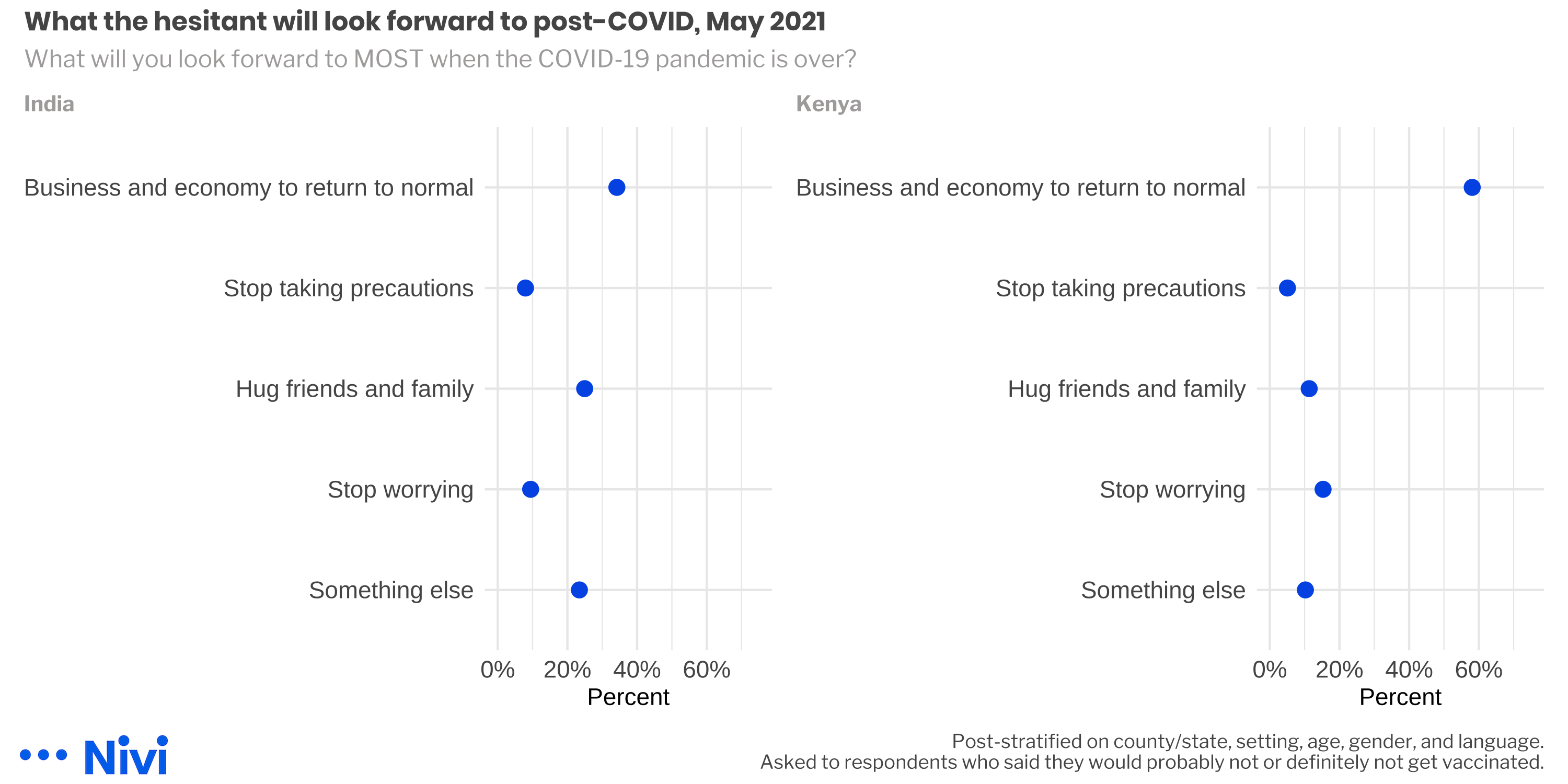
Figure 10: What the hesitant will look forward to post-COVID, May 2021
Network Effects
Approximately two-thirds of respondents in Kenya and India who have been vaccinated, or said they are willing to get vaccinated, told us that they have a friend or family member who is hesitant.
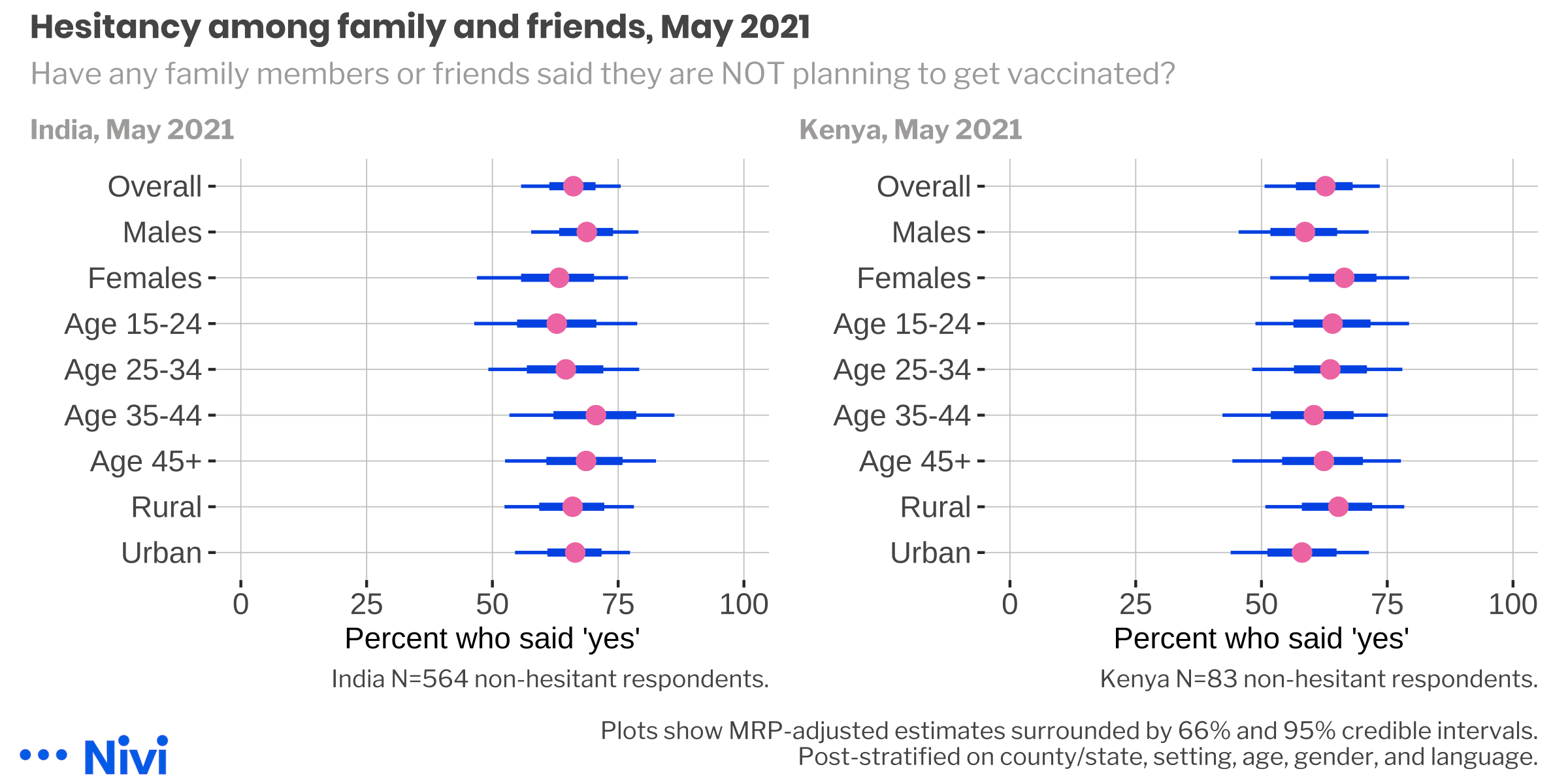
Figure 11: Hesitancy among family and friends, May 2021.
Interestingly, fewer than half of these respondents said that they have tried to convince their reluctant friends and family members to take action.
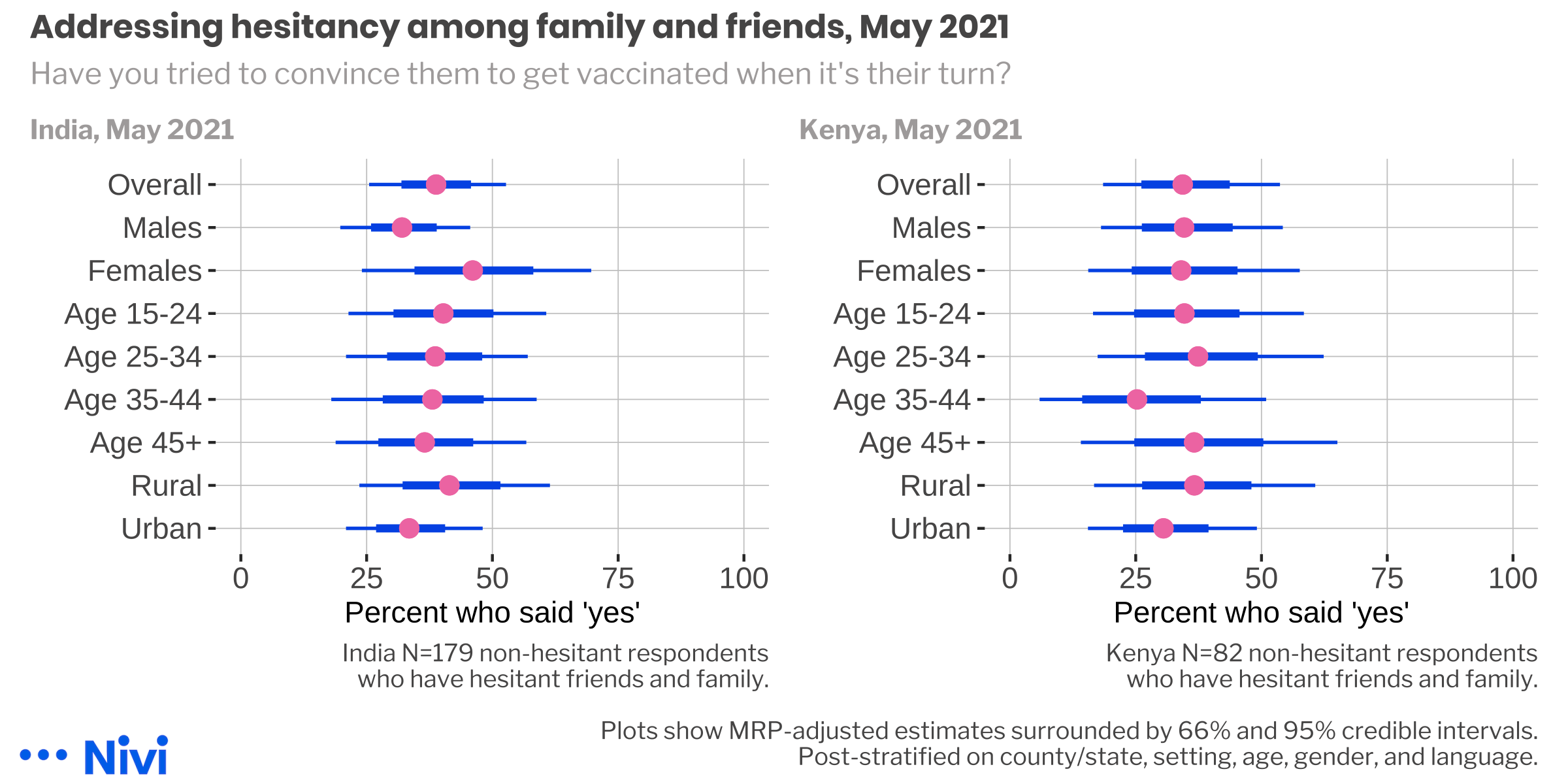
Figure 12: Hesitancy among family and friends, May 2021.
Half of the Kenyans who said they have not talked with their hesitant friends and family about vaccination attributed this to a lack of knowledge about how to have these conversations. This reason was less prevalent in the Indian sample where respondents were equally likely to say that these people would not listen, or that it was not their business to give advice.
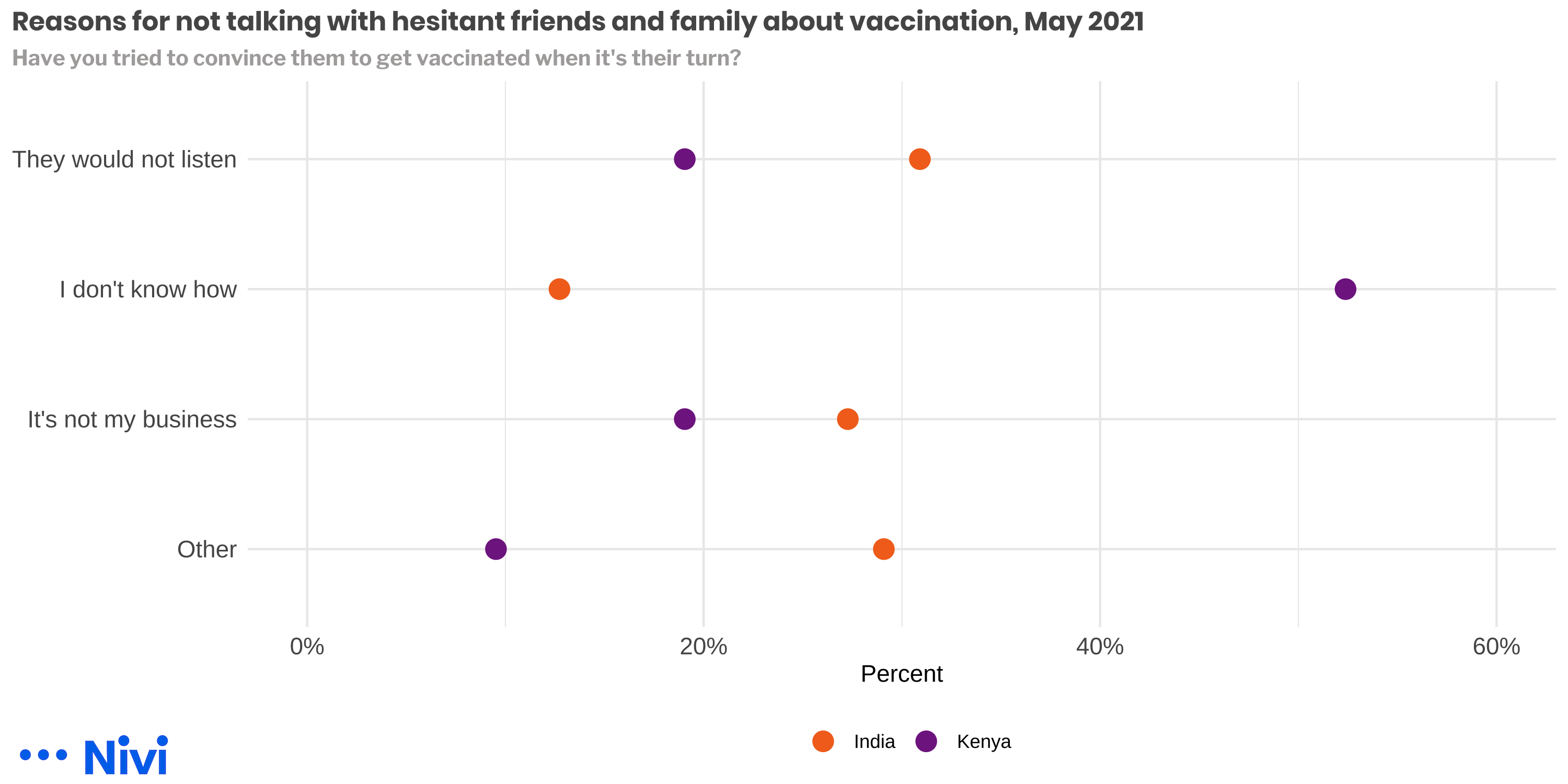
Figure 13: Reasons for not talking with hesitant friends and family about vaccination, May 2021
Promoting Behavior Change
There are three main barriers to vaccination:
- practical issues like cost, transportation, access that make it hard for people to get vaccinated, even if they want to;
- an individual’s negative beliefs and opinions about the safety, efficacy, and need for vaccines; and
- social contexts (social norms, social networks, social dyads) that are hostile to vaccination take-up.
, based on @brewer2017.](model.png)
Figure 14: The ‘Increasing Vaccination Model’, based on Brewer et al. (2017).
Brewer et al. (2017) review the vaccine behavior change literature and conclude that interventions that address the practical barriers to vaccination have the largest effects and strongest empirical support. For instance, mobile vaccine clinics in low-income neighborhoods can make it easier for people who might otherwise skip or delay vaccination because they have to work or cannot get a ride. These types of interventions are great for helping people who want to get vaccinated but face barriers to acting.
Another approach is to increase a person’s motivation to get vaccinated in the first place. The evidence for these interventions is weaker, but the challenge of COVID-19 demands a second look.3
While there is substantial work showing that understanding disease risk is correlated with getting vaccinated, and conversely that worries about side effects are correlated with not getting vaccinated, few trials have shown that interventions to change people’s beliefs have an impact on their actual vaccination behaviors (Brewer et al. 2017). However, even small effects delivered via new digital health interventions could be very cost-effective given the ubiquity of mobile phones and low communication costs.
Similarly, it is an open question whether social interventions can increase vaccine take-up. We are particularly interested in the potential of working through pro-vaccine people to influence the vaccination behaviors of individuals in their social network.
Take Kenya for example. We found that two-thirds of pro-vaccine adults in our survey have friends or family members who are hesitant to get a COVID-19 vaccine. Amazingly, fewer than half of these people said they had tried to intervene! The most common reason? They did not know how to start the conversation. We think askNivi can help.
Technical Notes
A concern with any convenience sample is that the results will be biased and will not necessarily represent the target population, which in our case was adults in both countries. We attempted to make the results more representative through multilevel Bayesian regression and post-stratification. Post-stratification data came from the 2016 FinAccess household survey for Kenya and the 2015-16 Demographic and Health Survey for India. Covariates in the model included age, setting (rural/urban), county/state, gender, and an indicator for English language ability.
For the May 2021 round, we also adjusted some responses for COVID-19 vaccination status after noticing that our sample was more likely than the respective target populations to have received a COVID-19 vaccine. To adjust the India data, we used Harvard University’s India COVID-19 Vaccine Tracker, which pulls from India’s COVID-19 Vaccine Intelligence Network (Co-WIN) system, to calculate the proportion of adults vaccinated at the time of the survey by state and age group. We then grouped the DHS data by age and state and used the relevant proportions to randomly generate a vaccination indicator. This enabled us to calculate reasonable cell proportions for stratifying based on vaccination status and the other covariates. To adjust the Kenya data, we used vaccination data from the Kenyan Ministry of Health and followed the same procedure (age breakdowns not reported).
This is an interesting example of the limits of survey post-stratification. Even after adjusting for gender, age, setting, county/state, and language, our survey estimates of COVID-19 vaccination status were ~10 percentage points higher than what officials were reporting for India and ~15 percentage points higher than the official Kenyan rate. We were able to further adjust other survey data based on vaccination status, but it is a reminder that recruitment still matters. The people who responded to our Facebook ads were more likely than the average adult to have been vaccinated. To the extent that we did not capture the views of certain segments of the target population, our results will still be biased. The post-stratification techniques we used help with the bias that can result from imbalances among the segments we did capture, but it does not account for selection bias.
Get in Touch
Let us know how we can put askNivi to work for your organization. Contact Ben Bellows at [email protected] with questions or to learn more.
India started vaccinating healthcare and frontline workers in January and expanded access to anyone over the age of 18 on May 1. As of today, more than 150 million Indians have received at least one dose of a COVID-19 vaccine, making India a close second to the United States. While this is an impressive number, it only represents approximately 10% of the overall population (15% of adults). Most residents remained susceptible as the virus spread uncontrolled in April and pushed health systems to the brink. Kenya began to distribute COVID-19 vaccine doses to priority groups in March, just as cases rose for the third time. This was not a wave of widespread suffering as in India and elsewhere, but many residents were subjected to new lockdowns and daily life was interrupted.↩︎
Kenyan ads were presented in English, while Indian ads were presented in Hindi. ~10% of respondents in each county opted to complete the poll in a language that differed from the language of the ad copy.↩︎
Also, most of the evidence comes from studies of children in high-income countries.↩︎